Juvenile myositis (JM), including juvenile dermatomyositis (JDM) and juvenile polymyositis (JPM), is a group of rare autoimmune diseases in which the body’s immune system attacks its own cells and tissues. Weak muscles and skin rash are the primary symptoms of JDM, while muscle weakness without a rash is the primary symptom of JPM.
JM affects every child differently. Some children experience a mild form of the disease, while others follow a more severe course.
We invite you to get to know some of our patients in our stories of hope.
Incidence of Juvenile Myositis
JM is a rare disease, and its exact incidence is unknown. Approximately two to four children in a million are diagnosed with JM each year in the United States.
JM begins in childhood or the teen years. The average age of onset for JM is between six to seven years old; 25% of diagnosed children are age four or less.
JM affects girls twice as often as boys. Once a child is diagnosed with JM, it is always considered to be the juvenile form, even if the patient continues with the disease into adulthood.
A skin rash is often one of the initial symptoms of juvenile dermatomyositis, preceding or accompanying a weakening of the stomach, neck, quadricep, or bicep muscles.
The Genesis of the Disease
The immune system is a group of cells that normally protects the body from infection and other environmental factors. In an autoimmune disease like JM, however, the body’s immune response is activated and doesn’t shut itself off. The immune system then mistakenly attacks previously healthy tissues (muscle and skin in JM), harming the body instead of protecting it.
The process that occurs when the immune system attacks healthy tissue is called inflammation. In JM, the inflammation primarily occurs in the blood vessels under the skin and the muscles, and this inflammation causes weak muscles and skin rashes. If blood vessels or muscle cells in other body parts are inflamed, other body systems can be affected, such as the digestive tract, heart, and lungs.
What Causes JM?
Researchers believe a convergence of environmental and genetic factors causes juvenile myositis. Children who develop this disease may have a family history of other autoimmune diseases, including thyroid disorder, type I diabetes, rheumatoid arthritis, lupus, or Crohn’s disease.
Juvenile myositis is a heterogeneous disease, presenting differently in each child and can be triggered by an array of genetic or external environmental factors.
If a child is genetically predisposed to JM, experts suspect that a virus or bacteria might trigger a runaway immune response that causes the body to attack itself. Other environmental factors, such as a heavy dose of sun exposure, may also play a role.
What Are the Symptoms of JM?
The primary symptoms of JM are weak or painful muscles, skin rash, fatigue, and fever. Some children experience joint pain as well.
Weak Muscles
The muscles most affected are near the body’s trunk: the stomach, thigh, neck and upper arm. Other muscles, however, can become weak as well. Sometimes there is inflammation in the swallowing tube or esophagus, which makes it difficult for the child to swallow. Other times, there is inflammation in the intestinal tract, which causes bowel difficulties and stomach pain.
A child with JM has difficulty climbing stairs and getting up from a sitting position. Walking and running become very challenging and exhausting. Some children will roll out of bed because sitting up and lifting the head becomes too difficult. In addition to weakness, some children with JM experience muscle pain.
Skin Rash
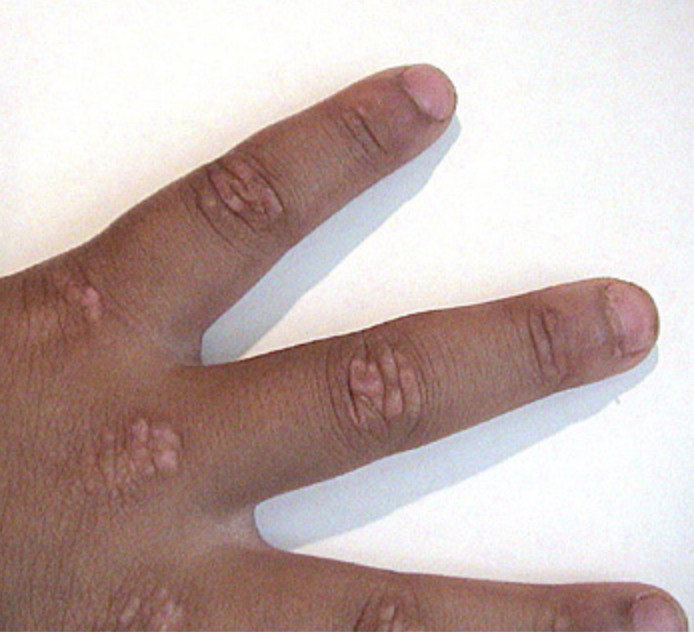
The skin rash in JDM usually occurs on the eyelids, knuckles, elbows, knees, and ankles. The rash may appear before, after or simultaneously as muscle weakness, and sometimes the rash is so faint that it is not noticeable.
The rash appearing on the eyelids is red and purplish and is referred to as a heliotrope rash, named after a flower of the same color. Another rash that frequently occurs on the cheeks takes on a red color and looks very similar to a sunburn.
On the knuckles, elbows and knees, the rash forms patches of red and scaly skin called Gottron’s papules. The fingernails and the nail beds may also take on a pinkish color.
Examples of rashes:









Fatigue
With JM, the child becomes tired easily and can only walk short distances. The child needs to rest often and lacks the energy for normal activities, making it difficult to keep up with friends.
Fever
Sometimes, the child with JM runs low-grade fevers, especially at night.
What Tests Are Used to Diagnose JM?
A doctor will perform a complete physical exam, specifically looking for rashes and muscle weakness. If JM is suspected, blood tests are the next step in making a diagnosis. Muscle enzymes, including creatine kinase (CK), aldolase, lactate dehydrogenase (LDH), aspartate aminotransferase (AST), and alanine aminotransferase (ALT), are measured.
If these lab tests are elevated, enzymes leak from inflamed or damaged muscles into the bloodstream. Antinuclear antibodies (ANA) are also measured to see if the child’s body produces antibodies against its own cells. Several myositis-specific autoantibodies have also been identified, which can be tested. Other blood tests are sometimes available to check immune activation and/or blood vessel damage. The next step in diagnosing JM is usually an MRI that detects muscle inflammation and damage.
A muscle biopsy may be performed to finalize the diagnosis if the MRI shows evidence of diseased muscles. When the characteristic rashes are absent, a muscle biopsy must be performed to exclude other causes of muscle weakness. A small amount of muscle is removed for examination under a microscope to determine if and how much the disease affects the muscles and blood vessels.
What Is the Treatment for JM?
Although medications can help alleviate the symptoms of JM, the disease has no known cure. The primary medications used to treat the symptoms of JM are corticosteroids, immunosuppressants, and chemotherapy. These medications can cause severe side effects, making JM challenging to treat. Many researchers believe that early and aggressive treatment is usually the best predictor of a better outcomefor this disease.
High-dose oral Prednisone or other corticosteroids, often coupled with intravenous corticosteroids and Methotrexate, are usually the first line of treatment for JM. Since the side effects of corticosteroids can be severe, Methotrexate, a chemotherapy drug administered at much lower doses than used for cancer patients, is usually introduced early to allow for tapering of the corticosteroids.
Second-line treatments are often considered as alternative treatments to allow patients to wean off of the steroids and methotrexate, or as an additional therapy if the first-line treatments are not sufficiently controlling the disease.
Common second line treatments include Intravenous Immunoglobulin (IVIG), Hydroxychloroquine (Plaquenil), Rituximab (Rituxan), Mycophenolic Acid or MMF (brand name CellCept or Myforic). Others may include Cyclosporine, Tacrolimus (Prograf), or Azathioprine (Imuran).
Some additional options that you may want to discuss with your doctor include Abatacept (Orencia), Tofacitinib (Xeljanz), TNF inhibitors, Tocilizumab (Actemra), Anakinra (Kineret), and Sifalimumab.
In addition, if you are dealing with calcinosis (a complication of JM), you might discuss with your doctor possible treatments for calcinosis including sodium thiosulfate (an IV treatment for calcinosis being studied at the NIH) and bisphosphonates (which has had some effects at reducing calcium deposits).
We know that JM is different for each patient, so always discuss your options with your doctor.
In addition, you may discuss with your doctor the importance of exercise, nutrition, quality sleep, protection from UV sunlight (sunblock and sunscreens), and vitamin D and calcium supplements.
Hear more about second line treatments in our “Ask the Doc” series at https://www.curejm.org/understanding-second-line-treatments-and-side-effects/
What Is the Prognosis?
There is no cure for JM yet, but with advances through research, early diagnosis, and aggressive treatment, outcomes for children with JM have continued to improve. JM is a heterogeneous disease, meaning the causes, symptoms, and long-term effects will differ among children. Some children experience a mild form of the disease and may go into medical remission within a few years of starting treatment. Others may have a longer seven to ten-year average course of treatment to achieve remission, and a smaller subset will follow a more chronic course that can require life-long maintenance therapies.
Research has led to earlier diagnoses and interventions, effective treatment protocols, and increased expertise among doctors in providing medical care. The mortality rate for JM patients has plummeted to less than 3% due to this research and medical progress. Much of this progress has been funded by the Cure JM Foundation in our 20-year history.
Many, if not most, JM children can look forward to a healthy future with their JM either in remission or managed through a moderate maintenance drug regimen.
Read our stories of hope.
Find a Doctor
Pediatric rheumatologists most often treat juvenile myositis at children’s hospitals. View Cure JM’s Clinical Care Network to find medical professionals who offer experienced care for JM. While the Network does not include every experienced physician qualified in JM care, we add to it yearly. If you don’t see a children’s hospital near you, email us at Info@curejm.org for additional information.
Myositis and You
For more detailed and comprehensive information about JM, please read the book, Myositis and You. This book was funded by the Cure JM Foundation and features over 450 pages with contributions from more than 80 experts and medical professionals. Receive a free digital copy when you join Cure JM.